
Shared Sacrifice
Chad Longpre Shepersky repeatedly took COVID-19 tests—and waited on pins and needles for results each time—during a coronavirus outbreak at Guardian Angels Health & Rehabilitation Center in Hibbing, Minn.
Longpre Shepersky, a certified nursing assistant (CNA), never contracted the virus. But he watched in agony as dozens of his patients and co-workers fell ill and fought for their lives.
As a weary nation enters the holiday season, Americans have an opportunity to help health care workers like Longpre Shepersky and start bringing the raging pandemic under control.
Consistently wearing face masks, practicing social distancing and taking other safety precautions will slow COVID-19’s spread and provide much-needed relief to the front-line workers battling burnout as well as the virus.
“Everyone should do their part,” insisted Longpre Shepersky, financial secretary and steward for United Steelworkers (USW) Local 9349, which represents workers at Guardian Angels. “Just the other day, I witnessed people in Walmart not wearing masks or following 6-foot distancing. Too many people aren’t doing what they can to fight the virus.”
As infection rates soar to their highest levels nationwide, the 10-month-old pandemic continues to take a disproportionately deadly toll on frail, vulnerable nursing home residents and the people who care for them.
So many residents and workers at Guardian Angels contracted the virus that the Minnesota National Guard last month sent a five-person team to help keep the 90-bed facility operating. Even then, as he worried about his own safety and mourned the deaths of several patients, Longpre Shepersky logged grueling amounts of overtime to fill in for ill colleagues.
“It got to the point where you dreaded going to work because you didn’t know what the day was going to bring,” recalled Longpre Shepersky, a CNA for 21 years who considers his co-workers and patients a second family. “But there was no one else there to do it. I just pulled up my Big Boy pants and went in to work and got through the day.”
Many nursing home workers endured staffing shortages at their facilities long before the pandemic. Because of low Medicaid payments for patient care, among other reasons, facilities paid low wages, skimped on staff or battled chronic turnover.
When COVID-19 struck, turnover and staff sicknesses compounded the chronic understaffing.
Now, nursing home workers struggle to stay physically and psychologically healthy while putting in extra shifts to ensure residents receive the highest quality care 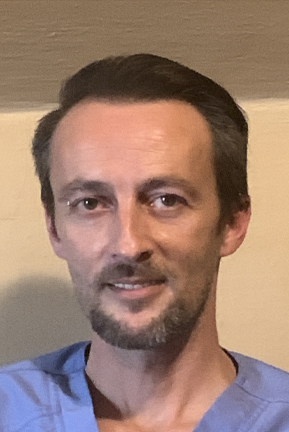 around the clock. Besides longer hours, many also took on additional responsibilities, such as serving as surrogate family members to residents cut off from visitors during facility lockdowns.
around the clock. Besides longer hours, many also took on additional responsibilities, such as serving as surrogate family members to residents cut off from visitors during facility lockdowns.
These everyday heroes feel stretched to the breaking point. Many nursing home workers and other health care professionals report unprecedented levels of burnout and other mental health concerns as they worry not only about their own safety but the fate of their patients and the possibility of bringing the virus home to their own family members.
“I try to go in with a positive mindset,” explained Shirley Richardson, unit president for USW Local 7898, which represents workers at the 220-bed Veterans’ Victory House in Walterboro, S.C. “The main object is being safe. I try to stay focused. I don’t let little things get to me.”
“It’s going to get better,” she reminds co-workers who’ve endured about two dozen cases of COVID-19, including the deaths of several patients and a nurse, at their facility. “This can’t go on forever. We just have to work through it.”
The pandemic highlighted the essential work that nursing home staff members perform—and the necessity of treating them as essential workers from now on.
That will require fixing the nation’s health care system—even if that means allocating additional tax dollars—so that nursing homes receive adequate payment for their services. Then the facilities can hire and retain adequate numbers of workers—and provide hazard pay and paid sick leave to ensure staffing remains at high levels during emergencies.
“It’s just the staffing that’s been the worst part of this year,” explained Chris Sova, unit president for USW Local 15301-1, which represents nurses at Bay County Medical Care Facility in Essexville, Mich.
“I feel like a zombie almost. I honestly don’t know how we do it anymore,” marveled Sova, a third-generation nursing home worker, who described his routine some weeks as “wake up. Go to work. Come home. Wake up. Go to work.”
It infuriates Sova to know that while he and his co-workers put their lives on the line every day, some Americans refuse to take simple steps to slow the virus’ spread.
Across the country, some people fail to wear masks even as infection rates in their own communities skyrocket and strain the capacity of local hospitals.
So far, at least 249,000 Americans died of COVID-19, more than 65,000 of them in nursing homes. Universal mask wearing, according to one new study, could prevent 130,000 more U.S. deaths in coming months.
“People wear seatbelts, but they have a big thing about facemasks?” Sova fumed.
Longpre Shepersky faces the upcoming holidays with trepidation, realizing that the family gatherings and parties Americans long for so earnestly this year also present additional opportunities for spreading the virus.
The residents at Guardian Angels wear masks whenever they leave their rooms, and because of the risk of another outbreak, they also could face limits on visitors this holiday season.
If they can make sacrifices to help contain the virus, other Americans can as well.
“Everyone definitely has to take this seriously,” Longpre Shepersky said.
*
Photo of Chad Longpre Shepersky
By clicking Sign Up you're confirming that you agree with our Terms and Conditions.
Related Blogs
Ready to make a difference?
Are you and your coworkers ready to negotiate together for bigger paychecks, stronger benefits and better lives?

