USS Proposed Health Network Would Limit Access to Providers, Increase Costs for Most Vulnerable
US Steel has proposed several changes in the health care plan which threaten to reduce your benefits and access to health care.
Proposal Restricts Specialty Drugs Under Medical Program
The Company proposes to eliminate coverage for high-cost Specialty Drugs obtained through a physician, clinic or infusion center, requiring all such Specialty Drugs to go through the Accredo Specialty Drug Program. Accredo would make certain decisions its own, regardless of physician input. This could disrupt the access of employees or family members with serious medical conditions to getting specialty drugs.
Controversial SaveOn Specialty Drug Program
U.S. Steel also proposes to implement the controversial SaveOn drug program, which would reduce plan reimbursement (increasing employee coinsurance) for certain high cost specialty drugs, unless an employee enrolls and applies for copay assistance programs through a drug manufacturer. At least one drug manufacturer has sued SaveOn for fraud related to program.
USS Proposes Restrictive Medical Network with NO Out-of-Network Coverage
The current U.S. Steel Medical Program delivers medical benefits through a Preferred Provider Organization (PPO) managed by Blue Cross Blue Shield (BCBS). A PPO is a type of managed care plan in which a network of doctors, hospitals, laboratories, and other health care providers have agreed to provide services for a negotiated cost.
The current BCBS PPO network is a broad network which gives you the flexibility to choose providers inside or outside the network each time you need care. There are advantages to using in-network PPO providers: coverage is higher, providers agree to accept negotiated rates and not to bill you for charges in excess of negotiated rates and network providers will handle any pre-certification of an inpatient admission. But the choice is up to you and your family.
U.S. Steel has proposed to replace the current PPO network with a restricted network, with fewer hospitals and doctors, and no coverage for out-of-network providers (except in emergency). The Company states that 76% of employees have adequate access to providers under its restricted network and would be required to use the network. Overall 36% of the providers used by USS employees today and almost 50% of claims dollars are outside of the proposed network.
You work hard. Work in a steel mill, coke plant or iron ore mine is difficult and often dangerous. It takes its toll. You deserve access to quality, affordable health care for you and your family.
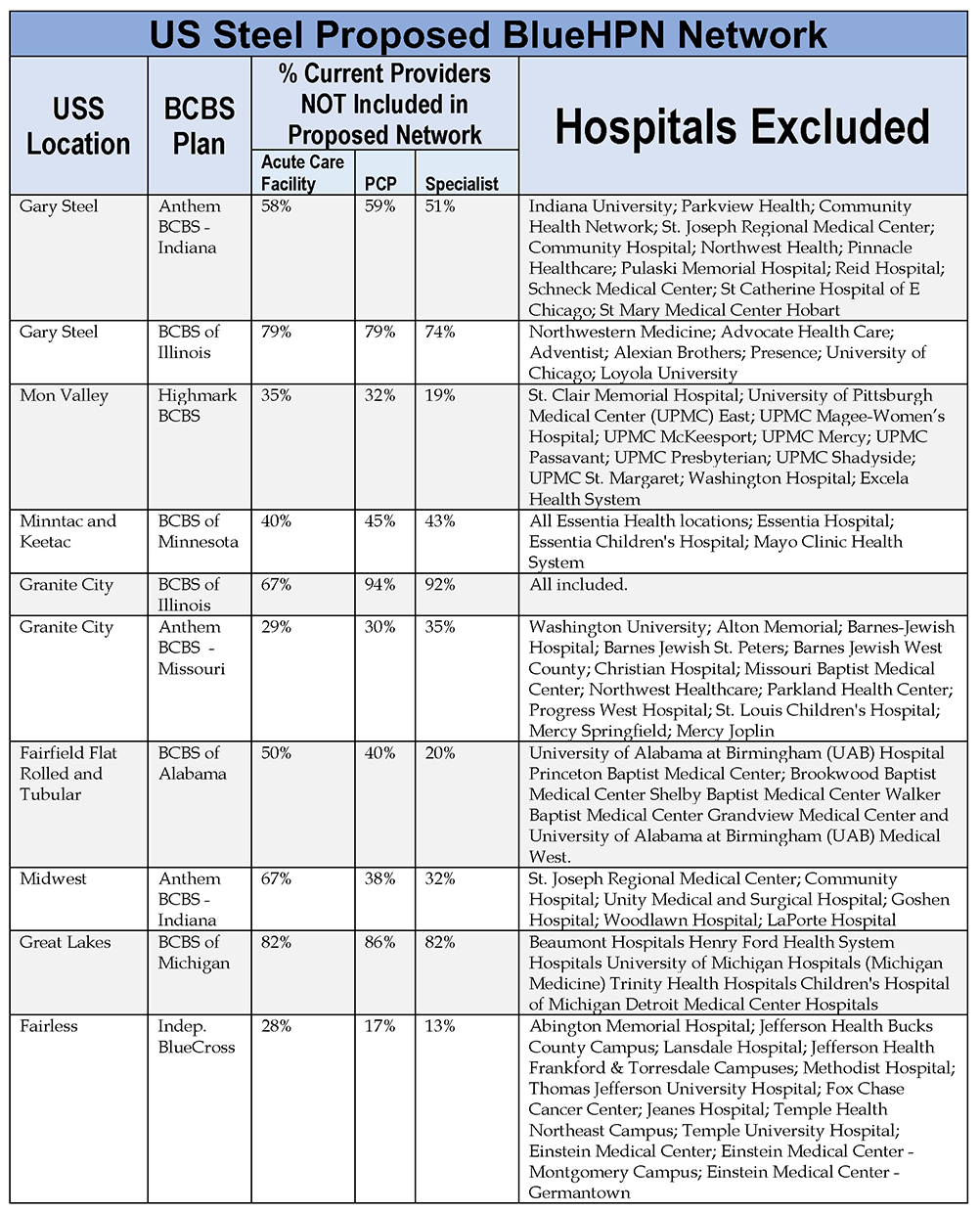
For example, the following table shows the share of providers available today through the BCBS BlueCard PPO network that would not be in the restricted network and not covered and the major hospitals that are excluded, except for emergencies, under the Company’s proposal: